Overview
Allergen immunotherapy offers a game-changing solution for allergy sufferers. This treatment exposes you to small amounts of allergens over time, helping your body build tolerance. It’s a beacon of hope for those living with chronic food allergies, including tough conditions like Chronic FPIES. Let’s dive into how it works.

Why Allergies Happen
Your immune system protects you from germs, but it can mess up. When you have allergies, it sees harmless stuff—like pollen or peanuts—as dangerous. This mix-up triggers symptoms: sneezing, itching, or worse, like trouble breathing.
A key player here is a protein called IgE. It spots the allergen and tells your body to release chemicals, like histamine, that cause those annoying or scary reactions.
The Science Behind Allergen Immunotherapy: How It Works
So, how does immunotherapy fix this? It’s like training your immune system to relax. You get tiny doses of the allergen—think peanuts or pollen—over months or years. Slowly, your body learns it’s not a threat.
This happens in two steps: - Build-up: Doses start small and grow bigger. - Maintenance: You keep getting steady doses to lock in tolerance.
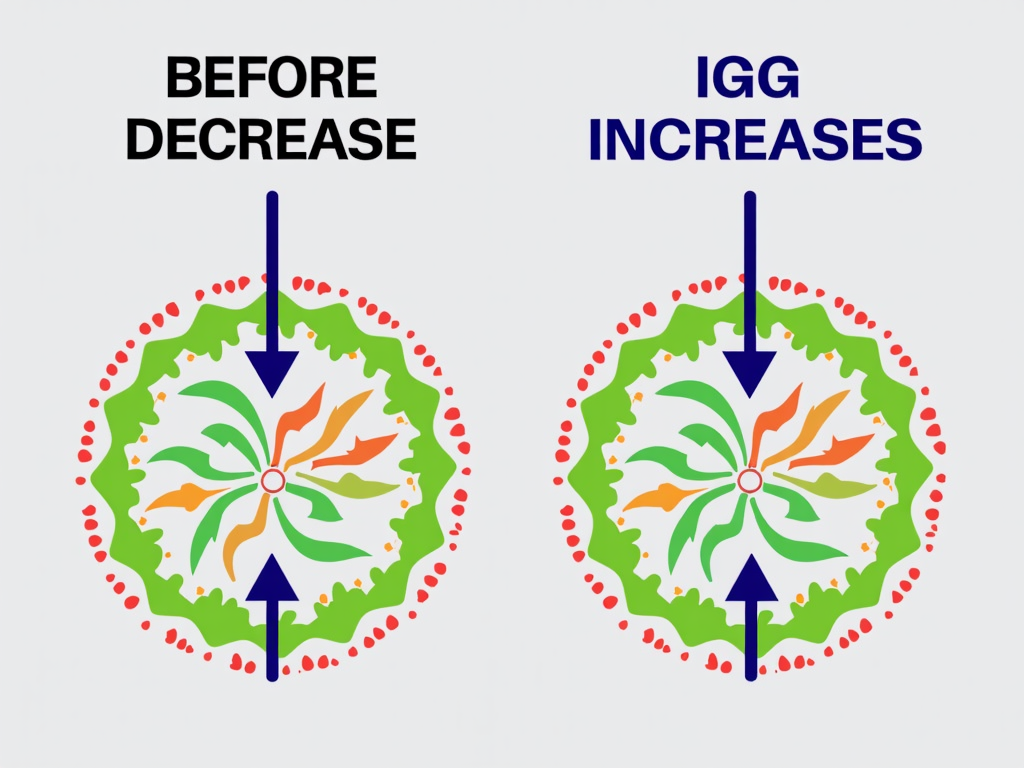
Scientists say it shifts your immune response. It boosts calmer proteins (IgG) and special cells (regulatory T-cells) that tell your body to chill out.
How You Get the Treatment
There are two main ways doctors deliver immunotherapy:
- Shots (SCIT): A nurse injects the allergen under your skin, usually in your arm. You start with weekly visits, then monthly.
- Drops or Tablets (SLIT): You place a tiny dose under your tongue. After a doctor’s okay, you can do this at home.
Both work well, but shots are common for food allergies, while drops suit things like pollen.
Does It Really Work?
Yes, studies back it up! Research from the Journal of Allergy and Clinical Immunology30922-6/fulltext) shows immunotherapy cuts allergy symptoms and medicine needs for many. For food allergies, a New England Journal of Medicine study found 67% of kids could handle peanuts after treatment.
It’s not risk-free, though. Some get mild swelling or, rarely, a big reaction. That’s why doctors watch you closely at first.

The Role of Allergen Immunotherapy in Modern Treatment
Today, immunotherapy is a big deal when pills or avoidance don’t cut it. For chronic food allergies, it’s a lifeline. Imagine not panicking over every bite! Even for rare conditions like Chronic FPIES—where food triggers vomiting or worse—it’s showing promise.
The American Academy of Allergy, Asthma & Immunology says it’s a long-term fix, not just a Band-Aid.
Living with Chronic Food Allergies
Life with a chronic food allergy is tough. You’re always on guard—reading labels, asking waiters, skipping parties. Kids miss out on cupcakes at school. Parents lose sleep worrying.
I’ve seen this firsthand. My cousin, Sara, couldn’t touch dairy without hives. Every outing was a gamble. Immunotherapy changed that. After two years, she enjoys ice cream—small scoops, but it’s freedom.

A Real Story: Jake’s Turnaround
Meet Jake, a 9-year-old with a peanut allergy. One whiff once sent him to the ER. His mom, Lisa, started him on shots after meds failed. It took 18 months—slow and steady. Now, Jake eats a few peanuts without a hitch. Lisa says it’s like getting her son back.
Not everyone gets this result, but for many, it’s a huge win.
What to Expect
Thinking about trying it? Here’s the scoop:
- Time: It’s not quick—months to years.
- Side Effects: Mild itching or swelling is common; serious stuff is rare.
- Cost: Insurance often helps, but check.
Talk to your doctor. For Chronic FPIES or other tricky allergies, research is growing, like this National Institute of Allergy and Infectious Diseases overview.

Wrapping Up
Allergen immunotherapy isn’t magic, but it’s close. It rewires your immune system to handle allergens better, offering relief for chronic food allergies and beyond. Whether you’re dodging peanuts or battling Chronic FPIES, it’s a science-backed path worth exploring. Ready to breathe easier? Check out more below!
Discuss Here