Food Protein-Induced Enterocolitis Syndrome (FPIES) is a serious but often misunderstood food allergy affecting infants and young children. Unlike typical food allergies, FPIES causes delayed gastrointestinal symptoms, making it challenging to diagnose. Early diagnosis is crucial to prevent unnecessary suffering, ensure proper management, and improve the quality of life for affected children and their families. This article explores the importance of recognizing FPIES symptoms early, discusses breastfeeding considerations, and provides insights into managing acute FPIES episodes.
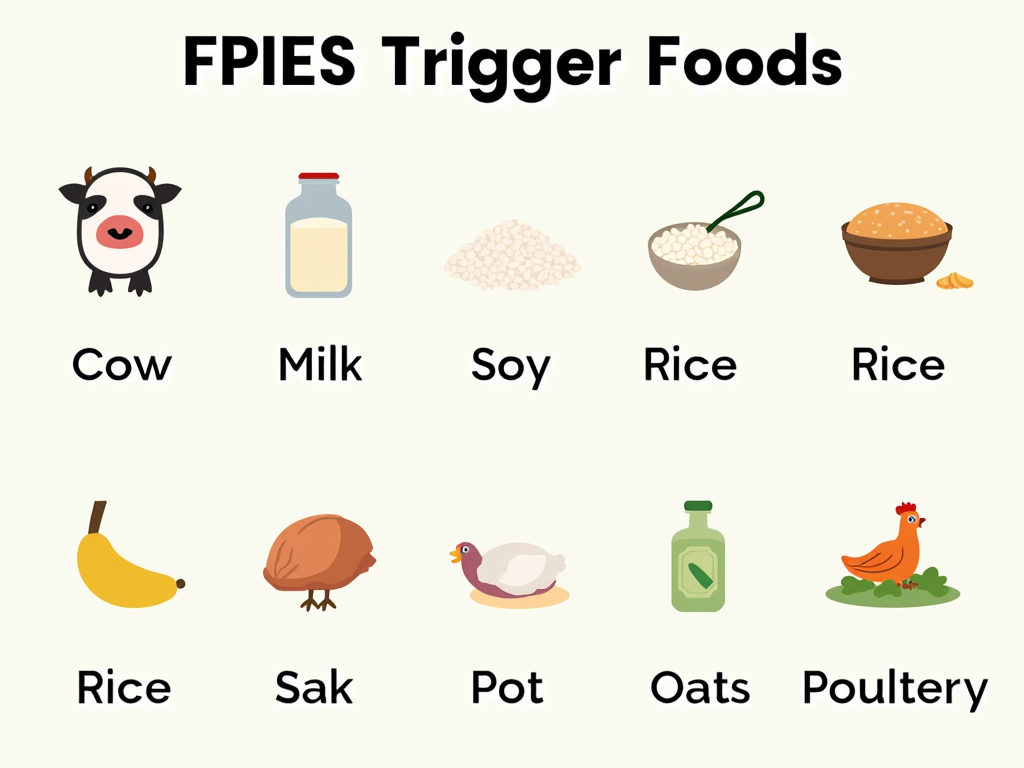
FPIES is a non-IgE mediated food allergy that primarily affects the gastrointestinal system. It typically occurs in infants between 2 and 7 months old but can also affect older children and, in rare cases, adults. The condition is triggered by certain foods, with the most common culprits being cow's milk, soy, rice, oats, and poultry. When a child with FPIES consumes a trigger food, their immune system reacts abnormally, leading to inflammation in the gut. This inflammation causes symptoms like severe vomiting, diarrhea, lethargy, and pallor, usually appearing 2 to 4 hours after ingestion. The exact cause of FPIES is unknown, but it's thought to be related to the immaturity of the infant's gut and immune system.
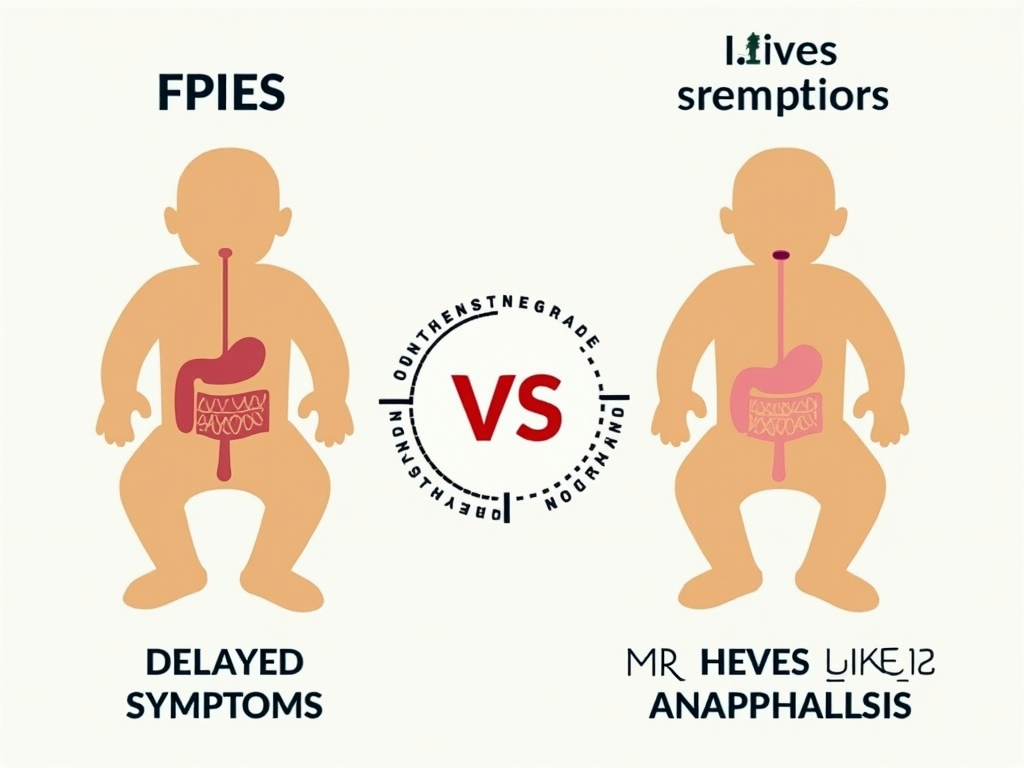
The hallmark symptoms of FPIES include: - Severe vomiting, often projectile, occurring 2-4 hours after eating the trigger food - Diarrhea, which may contain blood or mucus - Lethargy or extreme tiredness - Pallor or looking pale - In some cases, low blood pressure or shock-like symptoms Unlike IgE-mediated food allergies, FPIES does not cause immediate reactions like hives, swelling, or difficulty breathing. This delayed onset can make it difficult for parents and healthcare providers to connect the symptoms to a specific food. Additionally, FPIES reactions are dose-dependent, meaning that a small amount of the trigger food might not cause a reaction, but a larger amount will. Some children may also experience chronic symptoms like poor growth or irritability if they are repeatedly exposed to trigger foods.
Early diagnosis of FPIES is essential for several reasons: - Preventing Unnecessary Suffering: Without a diagnosis, children may continue to be exposed to trigger foods, leading to repeated episodes of vomiting and diarrhea. These episodes can be traumatic for both the child and the parents. - Avoiding Misdiagnosis: FPIES is often mistaken for other conditions such as viral infections, sepsis, or even surgical emergencies. Misdiagnosis can lead to unnecessary tests, treatments, and hospitalizations. - Ensuring Proper Management: Once diagnosed, families can work with healthcare providers to identify and avoid trigger foods, develop an emergency action plan, and monitor the child's growth and development. - Reducing Emotional Stress: The uncertainty and fear associated with undiagnosed FPIES can take a toll on families. Early diagnosis provides clarity and a path forward, reducing anxiety and empowering parents to manage the condition effectively. - Preventing Chronic FPIES: In some cases, repeated exposure to trigger foods can lead to chronic FPIES, where symptoms become more frequent and severe. Early diagnosis and avoidance of trigger foods can prevent this progression.
Breastfeeding is generally safe and beneficial for infants with FPIES. Breast milk contains antibodies and other factors that support the development of the infant's gut and immune system, which may help in managing the condition. However, if the mother consumes trigger foods, small amounts of the proteins can pass into the breast milk and potentially cause symptoms in the infant. Therefore, some mothers may need to eliminate certain foods from their diet. It's crucial to do this under the guidance of a healthcare provider or a dietitian to ensure that both the mother and the infant receive adequate nutrition. In most cases, breastfeeding can continue successfully with careful management.
During an acute FPIES episode, the child may experience: - Profuse vomiting, often leading to dehydration - Diarrhea, which can further contribute to fluid loss - Lethargy or unresponsiveness - Pallor or looking very pale - In severe cases, low blood pressure or shock If a child is having an acute episode, it's important to seek medical attention immediately. Treatment typically involves rehydration, either orally with electrolyte solutions or intravenously in a hospital setting. After the episode, parents should work with their healthcare provider to confirm the trigger food and adjust the child's diet accordingly. Long-term management includes strict avoidance of trigger foods and having an emergency action plan in place. This plan should outline steps to take during an episode, including when to seek emergency care and how to administer oral rehydration solutions.
Living with FPIES can be challenging, but early diagnosis can make a significant difference. One parent shared, "When my daughter was finally diagnosed with FPIES after months of unexplained vomiting, it was like a weight lifted off my shoulders. We could finally understand what was happening and take steps to protect her. Knowing the trigger foods and having a plan for emergencies gave us confidence and peace of mind." A pediatric allergist adds, "Early diagnosis of FPIES is critical because it allows us to implement dietary changes before the child experiences multiple severe reactions. It also helps in educating parents about the condition, which empowers them to manage it effectively and advocate for their child's needs."
Diagnosing FPIES can be tricky due to its delayed symptoms and similarity to other conditions. The gold standard for diagnosis is an oral food challenge, where the child is given the suspected trigger food under medical supervision and monitored for reactions. However, this should only be done in a controlled setting with emergency equipment available. Other diagnostic tools include: - Keeping a detailed food diary to track what the child eats and when symptoms occur - Ruling out other conditions through blood tests, stool tests, or imaging - Consulting with specialists such as allergists or gastroenterologists If you suspect your child has FPIES, it's important to work closely with your healthcare provider to get an accurate diagnosis and develop a management plan.
| Feature | FPIES | IgE-Mediated Food Allergies |
|---|---|---|
| Onset of Symptoms | 2-4 hours after ingestion | Immediate (within minutes) |
| Common Symptoms | Vomiting, diarrhea, lethargy | Hives, swelling, anaphylaxis |
| Diagnostic Tests | Oral food challenge | Skin prick test, blood test |
| Treatment | Avoidance of trigger foods, rehydration | Avoidance, epinephrine for emergencies |
The good news is that many children with FPIES outgrow the condition by the time they are 3 to 5 years old. However, the timeline can vary, and some children may have persistent allergies into later childhood or adulthood. Regular follow-ups with a healthcare provider are important to monitor the child's progress and determine when it's safe to reintroduce trigger foods. This process should always be done under medical supervision to avoid potential reactions.
Dealing with FPIES can be isolating, but there are resources available to help families. Support groups, both online and in-person, can provide a sense of community and shared experiences. Websites like the FPIES Foundation offer educational materials, research updates, and connections to medical professionals. Additionally, working with a dietitian who specializes in pediatric allergies can be invaluable for managing the child's diet and ensuring nutritional needs are met.
Early diagnosis of FPIES is essential for the well-being of affected children and their families. By recognizing the symptoms early, parents and healthcare providers can work together to manage the condition effectively. This includes identifying and avoiding trigger foods, understanding breastfeeding considerations, and being prepared for acute episodes. With the right support and information, families can navigate the challenges of FPIES and ensure a better quality of life for their children.
Discuss Here